Osteoarthritis
What is Osteoarthritis?
Cartilage tissue facilitates free movement of the joint with minimal friction. Damage or wear to cartilage tissue can lead to pain and may compromise the range of motion of the joint.
Osteoarthritis is the most common form of arthritic joint disease and is characterized by degenerative wear of the cartilage tissue that covers the inner surface of the joint. Osteoarthritis can present as a wide range of symptoms ranging from pain around the joint to stiffness and limited functional abilities.

What are the clinical features of Osteoarthritis?
The most common symptoms of osteoarthritis are pain, stiffness, and limited motion of the joint. Osteoarthritis might involve one joint or multiple joints. Hips and knees are joints that are commonly involved, but osteoarthritis can also affect the spine and hands and to a lesser degree, the shoulder, elbow, and the wrist. Symptoms of osteoarthritis typically appear in mid-life, but in rare cases can also appear in earlier years.
-
Sensitivity due to Osteoarthritis
Osteoarthritis can cause general discomfort and sensitivity, especially near the joint line.
-
Swelling due to Osteoarthritis
Osteoarthritis can cause swelling around the joint due to structural changes that occurs in the joint itself (osteophyte is an extra bone that grows on the sides of the joint and is a classic feature seen on x-ray of an osteoarthritic joint) and sometimes due to inflammatory flare up in the joint (proliferation of synovium which is an intra-articular tissue and extra fluid that accumulates inside the joint)
-
Limited motion due to Osteoarthritis
Osteoarthritis causes limited motion due to intra-articular tissue changes, such as osteophytes growth, condensed capsule that encloses the joint, synovial proliferation and extra fluid inside the joint. These anatomical changes can limit the range of motion of the joint.
-
Deformity and Osteoarthritis
Visible deformation of the joint can occur due to the above mentioned structural changes and tissue damage (degeneration of the cartilage tissue). This kind of deformation usually appears in advanced stages of osteoarthritis.
-
Instability and Osteoarthritis
Advanced osteoarthritis can cause joint instability due to muscle weakness and lack of confidence while walking.
Medical counseling for osteoarthritis
Initial diagnosis of osteoarthritis is usually carried out by an orthopedic doctor followed by a referral of the patient to a hip and knee specialist.
The specialist will ask the patient questions about the affected joint and following anamnesis, a physical exam is performed, and imaging is used to supplement the clinical findings.
-
X-ray for osteoarthritis diagnosis
X-ray is the most common imaging technique used for diagnosing osteoarthritis, it enables to identify the classic osteoarthritic imaging features such as narrowing of the joint space, osteophyte appearance and bone cysts. Correlation between the clinical findings and imaging results is important, especially in the early stages of osteoarthritis.

-
MRI
MRI is not typically needed for the diagnosis of osteoarthritis especially if the patient has representative symptoms and classic x-ray findings. MRI can show osteoarthritic changes in the joint even in early stages of the disease and intra articular structures that are not seen on x-ray, such as ligaments, menisci, synovium, and cartilage.
Knee Osteoarthritis
Knee osteoarthritis is the most common etiology to lower limb detriment in people over 50 years of age. From a structural point of view, the knee is divided to 3 compartments – medial (inner side), lateral (outer side) and patello-femoral (front side). The 2 most common compartments involved in osteoarthritis of the knee are the medial and patello-femoral. Pain in the inner aspect of the knee is characteristic to medial osteoarthritis while pain in the anterior aspect of the knee correlates with patello-femoral osteoarthritis. Patello-femoral osteoarthritis causes pain following sitting, changing position from sitting to standing and while ascending and descending stairs. (Descent will usually cause more pain due to extra stress on the joint). More extensive pain that radiates to the anterior aspect of the leg is common in moderate osteoarthritis and night pain is frequent in advanced stages of the disease. Osteoarthritis will typically not cause pain in the posterior aspect of the knee unless the patient has a popliteal cyst (a pouch with fluids that accumulates due to different etiologies such as a meniscal tear or osteoarthritis).
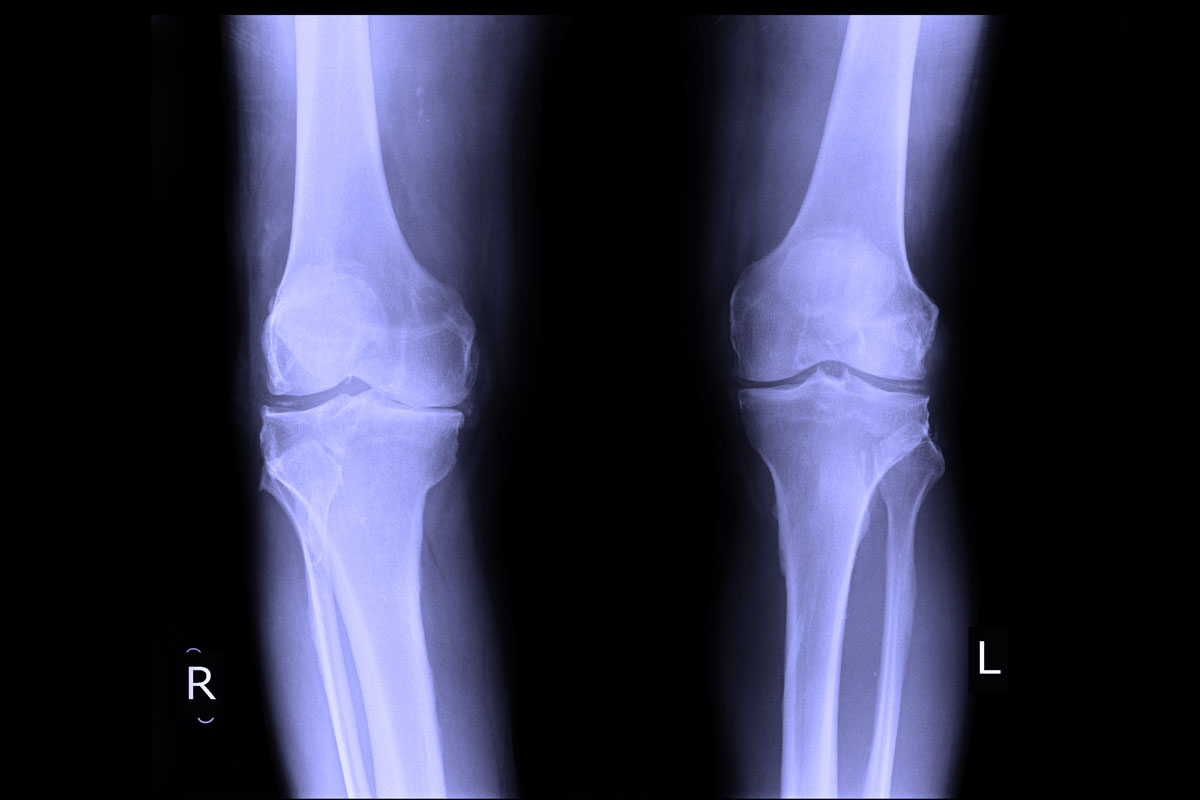
On the right side only mild symptoms of osteoarthritis are seen compared to the left where more advanced signs of cartilage degeneration are obvious.
Sometimes patients complain of instability of the joint and as if it ”gives way”, this is typical when there’s patello-femoral involvement and weakness of the quadriceps muscle, which can put the patient in danger of falling.
Hip osteoarthritis
Hip osteoarthritis causes pain, stiffness, and limited range of motion. Usually, the pain is around the groin area but might also involve the anterior-internal or the external-superior aspect of the thigh and even the buttock. Some patients might suffer from pain radiating to the thigh and the knee without having any symptoms around the hip joint itself. Pain gets worse when changing position from sitting to standing and while walking and running.
On physical examination, the patient might feel pain when rotating the joint and in advanced stage of the disease the leg is shortened and in an external rotation position. In some of the patients, more commonly in women, deterioration of osteoarthritis might be quite rapid, and the hip joint might degenerate in several months’ time.

In this pelvic x-ray on the right side a normal hip joint is seen, while on the left advanced signs of hip osteoarthritis are clear
Osteoarthritis treatment
The aim of treatment of osteoarthritis is pain relief and improvement of function. Treatment is divided into surgical and non-surgical (conservative).
Conservative treatment for Osteoarthritis
Generally, conservative treatment of osteoarthritis combines several approaches that might mitigate symptoms, including weight loss, physical exercise (beneficial both for muscle strengthening and aerobic endurance), physiotherapy (with an instructor) which are typically combined with several types of medications. No known medication can change the course of the disease; however, analgesics can be used to alleviate pain and anti-inflammatory drugs can be used to reduce inflammation. Intra-articular steroid injections might serve as a temporary solution over a short-term of several weeks as are hyaluronic acid injections.
Surgical treatment for Osteoarthritis
When conservative management is ineffective one should consider surgical treatment. Joint arthroplasty is the surgical treatment recommended for osteoarthritis and most of the patients that have total knee replacement or total hip replacement will see a marked increase in the quality of life. When considering surgical intervention multiple elements must be taken under consideration aside from the joint disease itself, like general health background, functional status, other joints that are involved etc. All of these altogether will have direct impact on the potential success of the surgery.

אשמח להשיב
מלאו את הפרטים מטה ואחזור אליכם בהקדם